The Quest for Sleep
Thursday, August 16, 2018
by Aimee Sterk, LMSW, MATP Staff
I first wrote this piece in 2013 and have dug it up to share again in honor of my respiratory therapist, David Gritter, retiring. He actually retired in May, but I was on maternity leave so I’m sharing this in my first post since returning. Dave is among a group of medical and helping professionals from a variety of disciplines that have come into my life and saved it. Because of him, I tried again to use devices to help me sleep. Because of him, I am no longer dangerously sleepy at the wheel. Because of him, I’m now an evangelist for sleep studies and have gotten at least one friend to go in (and find out she needed a CPAP too). Because of Dave, and my new sleep specialist physician Dr. Jason Coles, I am now using a BiPAP and I made it through four pregnancies, two losses, and IVF which all complicated my sleep. Because of them and their help and guidance, I get to partner with my husband to raise two beautiful kids and participate actively in the communities and work that I love.
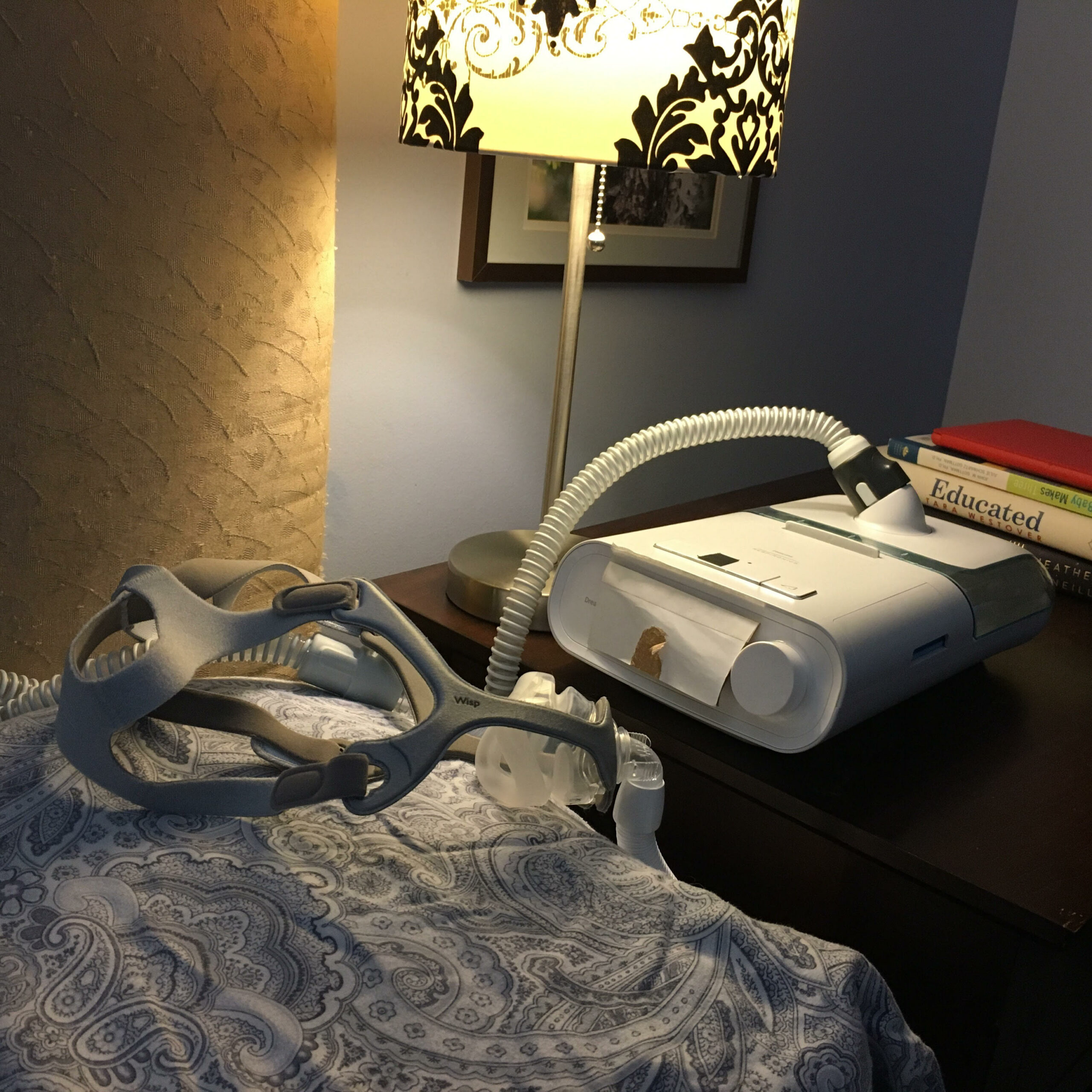
My trusty BiPAP and face mask which Dr Coles and Dave helped me get during my pregnancies when my air swallowing made my CPAP unusable for me. BiPAPs have two levels of pressure (lower pressure on the exhale) which helped make my air swallowing more manageable. I added the cardboard flap on the front to cover the bright light that comes on when you turn the machine on.
July 2013
I have been on a quest for good sleep for the better part of 8 years. I can remember having trouble sleeping even as a kid, but it didn’t affect my energy level during the day. As I age, the lack of energy is catching up with me. I sought help from a sleep specialist when my tiredness was affecting my ability to drive safely.
The first sleep specialist I saw didn’t believe my assertion that my hormonal problems (I have polycystic ovarian syndrome—PCOS) were related to my sleep. He discounted my feelings and my evidence and told me I needed a series of sleep studies and likely I was experiencing sleep problems as a result of clinical depression. I had clinical depression previously and knew I didn’t have it again. I didn’t appreciate the way he talked to me or his jump to diagnose or his statement that I needed many sleep studies for thousands of dollars to get to the bottom of this problem. I didn’t make a follow up appointment.
I did some research on my own, switched up some of my medications, and had some relief for a while, then, I again had trouble driving safely. I looked for a new sleep specialist.
The next sleep specialist I saw listened to me, believed me, and convinced me to have a sleep study.
The sleep study showed I have upper airway resistance syndrome (UARS). While not sleep apnea, it can produce similar disturbances in sleep. The brain waves from my sleep study also confirmed that I was not clinically depressed at that time.
I began the journey for ways to resolve UARS. After trying bite splints, consults for surgical options, sleeping in new positions, and fancy pillows that didn’t work, my sleep specialist convinced me to try a CPAP again (continuous positive air pressure) device.
I had given up on a CPAP before after difficulties with swallowing air. A previous respiratory therapist was dismissive of my complaints and I simply gave up. I wasn’t excited to try again. Just after a new respiratory therapist, Dave Gritter, came in the room, I burst into frustrated and defeated tears. I really didn’t believe this device would help me.
Dave was very patient and explained my sleep study to me in more detail, told me about research that showed CPAPs can be effective with UARS and also told me that new definitions of apnea were being developed and I did fit in the new definitions. He told me he truly believed that this device would work for me. He also explained that while some people notice a difference immediately, others take some time and/or don’t actually notice a difference until someone points out to them that they seem less tired. He encouraged me to try to rest and read while using the CPAP to get used to it and to take it off in the middle of the night if it was bothering me. He gave me a number to call if I had trouble.
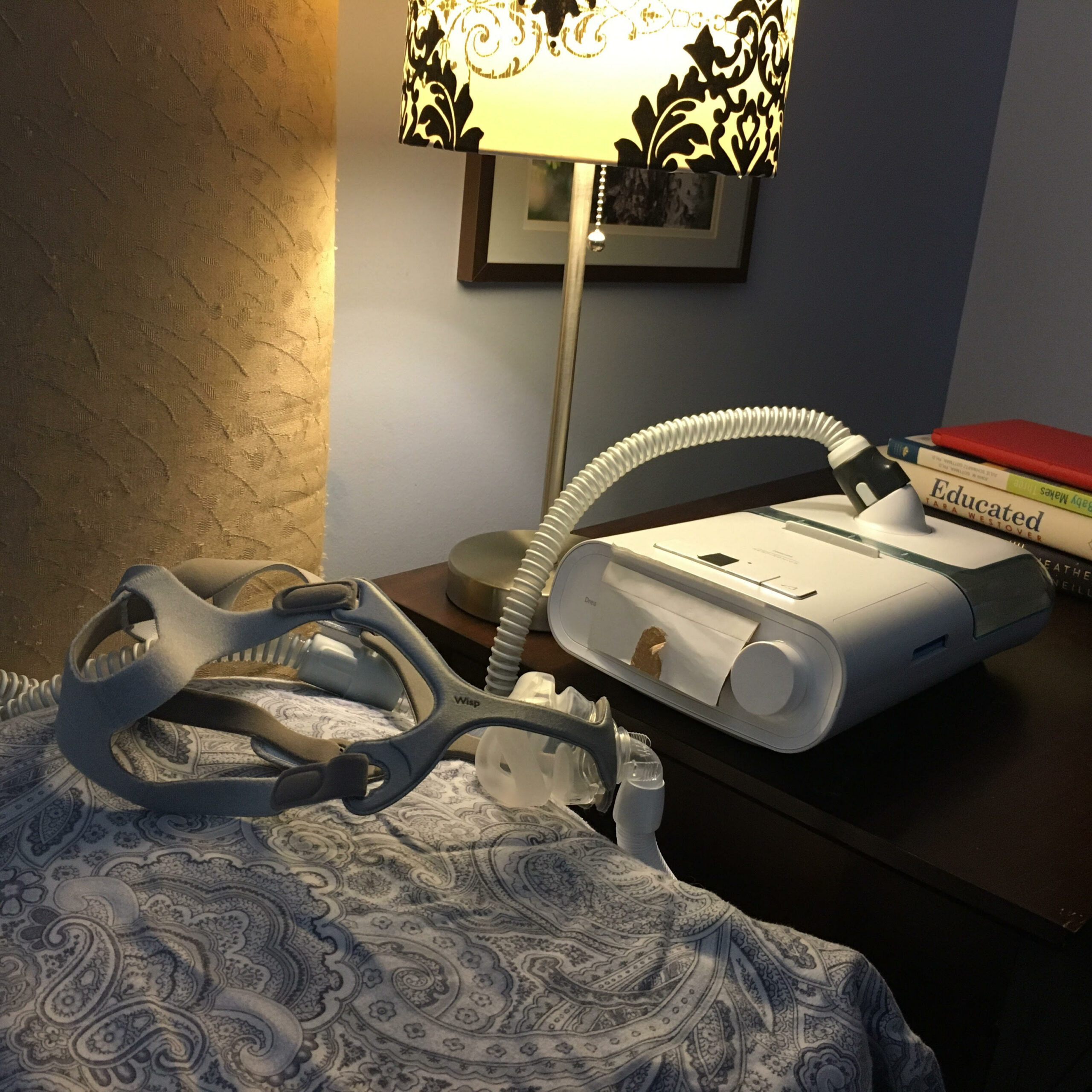
I started out on a very low pressure to see if it would work without causing me to swallow air. I still had lots of problems swallowing air, but with reassurance from Dave, I kept using the CPAP. I didn’t like how it made me look—like a strange astronaut—and

See?! Even the model looks like an astronaut (I’m still working on disability pride here, clearly), but this device and mask save my life every night.
was embarrassed to have to use it while staying at a friend’s house. My husband was supportive though. After 3 weeks, I noticed feeling much better during the day. I didn’t feel like I needed a nap and I no longer worried about falling asleep at the wheel. By two months in, I was using the CPAP all night and wrote a letter to Dave saying that the device was life changing.
Since that time, I have had ups and downs. I think they are related to hormone fluctuations and my other specialists have said that is something I have to live with.
While I wish I was well-rested and energetic all the time, as I was in the early months of using the CPAP, I’m still convinced that it helps me. I very rarely have trouble driving—a key sign to me that there is a problem. I used to have trouble driving every day.
I’m grateful for the journey I’ve been on. I knew myself, found health professionals that listened to me, believed me, and supported me to do what was best for me. I continue to look for ways to feel better but know that my disabilities present both gifts and barriers. I have learned a lot about good sleep habits, my own body, and how it functions, and the gifts of feistiness and noncompliance when dealing with health professionals who aren’t really on my team. I have found a piece of Assistive Technology that helps me do what I want to do—sleep. It’s not perfect, but it’s a good start.
Did you know that untreated sleep apnea takes years off of your life and that driving while drowsy is just as dangerous as drunk driving?
How have you advocated for yourself in the medical community to get to professionals that have helped?

